WHAT IS TMD?
TMJ is an acronym for “Temporomandibular Joint,” the joint that allows our lower jaw to open and close. We all have two TMJs: one on the right and one on the left. Malfunction of this complex joint mechanism on one or both sides is referred to as Temporomandibular Dysfunction/Disorder, or “TMD.” Many symptoms are associated with TMD, including:
- Dizziness
- Earaches
- Shoulder and back pain
- Jaw-joint pain
- Facial muscle tension
- Headaches
These common symptoms are often misdiagnosed and improperly treated using pain medication. Sometimes people suffering from TMD are told it’s all in their head, creating frustration and an ongoing search for a cure. The key to successful treatment is treating the cause of the pain rather than the pain itself. So, what causes TMJ pain?
HOW TMD IS RELATED TO MALOCCLUSION
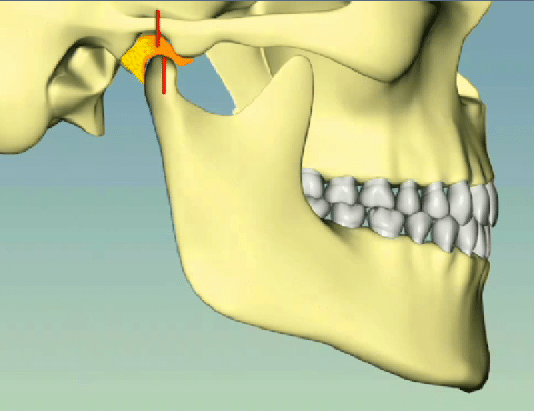
One of the most common causes of TMJ pain (“TMD”) is malocclusion, an improper fit of the lower teeth against the upper teeth. Occlusion is the term dentists use to describe how the teeth fit together, thus malocclusion translates to “bad-fit” or “bad-bite.” You may ask, “What do the teeth have to do with the jaw joints?” Your jaw joint—which holds your lower jaw in place—is suspended beneath your skull by an intricate system of muscles and tendons. The jaw joint is where the red line appears in the following diagram; the jaw muscles appear in blue or violet.
Fig. 1
The jaw joints and the groups of muscles that help stabilize and position the lower jaw are affected by the fit of the teeth. When the jaw is closed and the teeth fit together, the ball-shaped part of the lower jaw should fit into the socket-shaped part of the upper jaw (Fig. 2). If the lower jaw must be positioned out of the socket for the teeth to fit together, strain is put on both the jaw positioning muscles and the cartilage within the joint cavity (yellowish orange). This scenario is depicted in Fig. 3 where the red lines don’t line up. Think of when you must stand with your knees bent; your muscles must work to keep your weight supported, as opposed to standing with your knees locked where your muscles simply work a little bit to keep you balanced. Standing with knees locked is similar to Fig. 2, while standing with your knees bent is similar to Fig. 3.
Fig. 2—stable bite with jaw seated in socket
Fig. 3—unstable bite with jaw joint unseated in socket
The fit of the teeth affects the position of the lower jaw, which in turn affects the surrounding muscles that act to position and stabilize the lower jaw. By the same mechanism, the fit of the teeth also affect the cartilaginous “padding” between the upper and lower jaw called the “articular disc.” (The disc is yellow-orange in the figures above).
When this misalignment between teeth exists there becomes a subconscious shift of the lower jaw. The teeth may work just fine, however, there are usually signs of this malocclusion in the form of:
- Clenching
- Grinding
- Premature tooth wear
- Stress on muscles and tendons
- Distortion of the articular disc
The patient may be totally unaware of some of these signs, however, they often notice symptoms of TMD, such as:
- Headaches (caused by muscle tension)
- Muscle aches in the face, neck and upper back
- Facial pain
- Dizziness
- Earaches or ringing in the ears
- Pain directly from the jaw joint(s)
These symptoms are commonly, and sometimes unnecessarily, “treated” by prescribing pain medications and/or muscle relaxers. This is treating the symptom rather than treating the cause of the symptom, which is often malocclusion. How do we diagnose malocclusion, one of the most common causes of TMD?
DIAGNOSING MALOCCUSION
To accurately diagnose malocclusion we must know how the upper and lower teeth fit together when the lower jaw is in its “seated” position. Since the fit of the teeth can be affected by the health of the jaw joint, (bone resorption/malformation or disc displacement), a specialized radiograph of the jaw joints may be taken called a Cone Beam Computerized Tomograph (CBCT). In addition the dentist must make plaster models of the patient’s teeth and place them on a device called a “dental articulator” that closely simulates the patient’s jaw movement. A wax bite record made between the teeth while the patient’s jaw is in its seated position allows the dentist to accurately relate the lower teeth to the upper teeth on the articulator. By studying the patient’s bite on the articulator, the dentist can then see how the upper and lower teeth fit together without the interference of the patient’s reflexes and muscle tension holding the jaw into the position where the teeth fit. Remember, it’s this habitual posturing of the jaw into the position where the teeth fit that often creates the muscle and joint tension people notice when they have TMD.
TREATING MALOCCLUSION
Once the dentist finds there is malocclusion, they must determine the best way of treating it. The occlusion can be altered in several ways:
- Minor reshaping of the teeth (called “occlusal equilibration”)
- Movement of the teeth using orthodontic treatment (“braces”)
- Changing the length and/or width of the jaw(s) using oral surgery
- Changing the shape of the teeth using crowns
- Simply preventing the teeth from rubbing together, using an “occlusal splint”
- Any combination of the above
What we choose depends on many factors including but not limited to:
- The degree of malocclusion
- The condition of the teeth
- Age and health of the patient
- Patient’s goals for dental health
- Patient’s budget
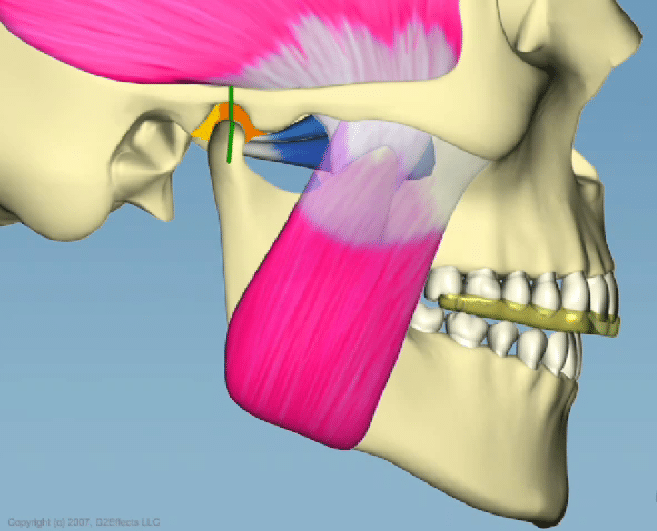
The simplest and least invasive way to treat malocclusion, without altering the teeth, is to fabricate an “occlusal splint.” There are many different designs of splints, however, they all have one thing in common: each splint is designed to reposition the lower jaw by separating the teeth. Keeping the teeth separated eliminates the muscle tension caused by the malocclusion and thereby eliminates the symptoms.
One common splint design is worn over the upper teeth. As it separates the teeth, the jaw is able to attain a resting position with the lower jaw up into the socket; with the teeth no longer “locking together” like gears, the jaw can slide up and back into this resting position. In addition, the muscles can relax, as they no longer need to stabilize the jaw in the position where the teeth fit together.
Fig. 4—an occlusal splint in place with the jaw joint seated
Even though one of the alternate methods of fixing malocclusion may be appropriate it’s usually best to start by trying a splint. Out of the five methods listed above, the splint is the only method that is completely reversible and requires no alteration of the teeth. All other methods, such as crowns or jaw surgery, are not reversible and may not always work. A splint is a great way to test how changes in occlusion affect the symptoms a patient is having before doing any permanent alterations in the mouth.
WHAT SHOULD I DO IF I SUSPECT I HAVE SYMPTOMS OF TMD/MALOCCLUSION?
The most important aspect of treatment is accurate diagnosis. No one wants to have unnecessary treatment; therefore it’s important that your dentist spends the time to find out what is causing your pain or discomfort. There are certainly other factors besides malocclusion that can cause symptoms similar to those of TMD. A good diagnostic process should rule out those potential sources of pain.